Challenges we solve
Keep Your People Safe and Connected

Your Emergency Communication Solution for Any Critical Event
Organizations need the ability to communicate quickly and effectively with employees during emergencies and other critical events. No matter what incident your organization faces, AlertMedia can help you keep your people safe, informed, and connected.
Respond Effectively to Any Event
-
 Desktop AlertsUse AlertMedia Desktop Alerts to deliver time-sensitive messages directly to employee screens.Learn MoreDesktop Alerts“By diversifying our communication channels, AlertMedia ensures we can always reach associates during critical events.”
Desktop AlertsUse AlertMedia Desktop Alerts to deliver time-sensitive messages directly to employee screens.Learn MoreDesktop Alerts“By diversifying our communication channels, AlertMedia ensures we can always reach associates during critical events.” Learn More
Learn More -
 Business ContinuityUse AlertMedia to reduce downtime, keep your critical operations going, and ensure your employees remain productive and safe—anywhere in the world, 24/7/365.Learn MoreBusiness Continuity"Threat Impact Assessment and Warnings provides an added layer of security for our business continuity plans.”
Business ContinuityUse AlertMedia to reduce downtime, keep your critical operations going, and ensure your employees remain productive and safe—anywhere in the world, 24/7/365.Learn MoreBusiness Continuity"Threat Impact Assessment and Warnings provides an added layer of security for our business continuity plans.” Learn More
Learn More -
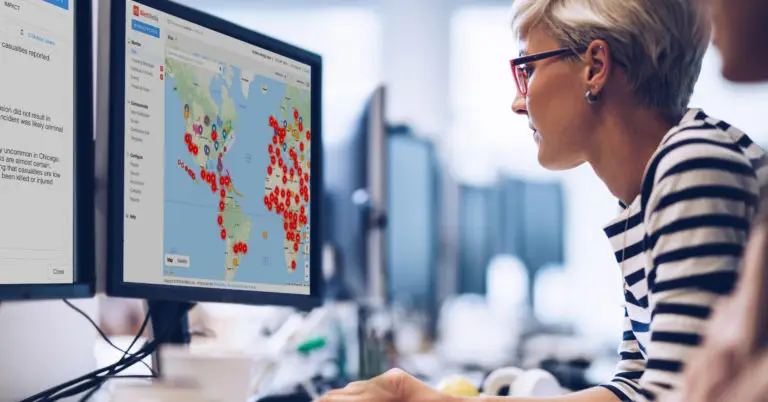
 Location and Asset ProtectionUse AlertMedia to gain real-time visibility into critical events happening anywhere you have people, locations, and assets.Learn MoreLocation and Asset Protection"AlertMedia’s threat assessment engine allows us to take the manual element out of threat monitoring and analysis, minimizing our exposure to risk and improving safety outcomes."
Location and Asset ProtectionUse AlertMedia to gain real-time visibility into critical events happening anywhere you have people, locations, and assets.Learn MoreLocation and Asset Protection"AlertMedia’s threat assessment engine allows us to take the manual element out of threat monitoring and analysis, minimizing our exposure to risk and improving safety outcomes." Learn More
Learn More -
 Emergency PreparednessUse AlertMedia to quickly identify threats and communicate with your employees faster during emergencies and other critical events.Learn MoreEmergency Preparedness“AlertMedia helps us make sure employees know we consider their safety a top priority and are prepared to protect them through any emergency."
Emergency PreparednessUse AlertMedia to quickly identify threats and communicate with your employees faster during emergencies and other critical events.Learn MoreEmergency Preparedness“AlertMedia helps us make sure employees know we consider their safety a top priority and are prepared to protect them through any emergency." Learn More
Learn More -
 Winter WeatherAvoid costly disruptions and ensure employee safety during severe winter weather.Learn MoreWinter Weather“We’ve used AlertMedia many times due to winter weather, and our HR team thinks it’s worth its weight in gold.”
Winter WeatherAvoid costly disruptions and ensure employee safety during severe winter weather.Learn MoreWinter Weather“We’ve used AlertMedia many times due to winter weather, and our HR team thinks it’s worth its weight in gold.” Learn More
Learn More -
 Return to WorkKeep employees informed and your business compliant with new workplace safety regulations.Learn MoreReturn to Work“With AlertMedia, JMI can reopen its offices responsibly and boost employee morale. We are pleased that we can start giving our employees the option to reenter the workplace if they are ready.”
Return to WorkKeep employees informed and your business compliant with new workplace safety regulations.Learn MoreReturn to Work“With AlertMedia, JMI can reopen its offices responsibly and boost employee morale. We are pleased that we can start giving our employees the option to reenter the workplace if they are ready.” Learn More
Learn More -
 California AB 685Comply with state regulations and keep employees informed about workplace incidents.Learn MoreCalifornia AB 685“AlertMedia has absolutely helped us meet the state’s requirements around reporting to work during the pandemic.”
California AB 685Comply with state regulations and keep employees informed about workplace incidents.Learn MoreCalifornia AB 685“AlertMedia has absolutely helped us meet the state’s requirements around reporting to work during the pandemic.” Learn More
Learn More -
 COVID-19Conduct daily health screenings and keep in touch with essential workers.Learn MoreCOVID-19“With AlertMedia, we can efficiently follow COVID-19 reopening guidelines, protect employee health and safety, and proactively assist employees that may be exhibiting symptoms.”
COVID-19Conduct daily health screenings and keep in touch with essential workers.Learn MoreCOVID-19“With AlertMedia, we can efficiently follow COVID-19 reopening guidelines, protect employee health and safety, and proactively assist employees that may be exhibiting symptoms.” Learn More
Learn More -
 HurricanesCommunicate critical information to impacted employees during all phases of a storm.Learn MoreHurricanes“The ability to quickly reach employees across multiple channels is critical during a hurricane when you may experience power outages.”
HurricanesCommunicate critical information to impacted employees during all phases of a storm.Learn MoreHurricanes“The ability to quickly reach employees across multiple channels is critical during a hurricane when you may experience power outages.” Learn More
Learn More -
 Remote WorkforceMonitor threats across multiple locations and protect your remote workforce.Learn MoreRemote Workers“Being able to identify who has received and read any given notification is invaluable to assessing employee well-being.”
Remote WorkforceMonitor threats across multiple locations and protect your remote workforce.Learn MoreRemote Workers“Being able to identify who has received and read any given notification is invaluable to assessing employee well-being.” Learn More
Learn More  Workplace FiresPrepare for and recover from fires in the workplace.Workplace Fires"I love the AlertMedia system. It is very flexible and allows me to have preset emergency templates that make it easy to send out an alert."
Workplace FiresPrepare for and recover from fires in the workplace.Workplace Fires"I love the AlertMedia system. It is very flexible and allows me to have preset emergency templates that make it easy to send out an alert."
 WildfiresMake at-risk employees aware of rapidly-changing safety risks.Wildfires“AlertMedia’s platform made it easy to isolate impacted employees, and quickly communicate with them based on location. ”
WildfiresMake at-risk employees aware of rapidly-changing safety risks.Wildfires“AlertMedia’s platform made it easy to isolate impacted employees, and quickly communicate with them based on location. ”
Equip Your Team to Navigate Any Emergency
We’ll help you communicate faster during any critical event
- Safety & Security
- Security threats
- Inclement weather
- Health risks
- Workplace hazards
- Facility issues
- Incident reporting
- Information Technology
- Outages
- Planned downtime
- System testing
- Cyberattacks
- Security breaches
- Escalations
- Human Resources
- Covid-19 screenings
- Wellness checks
- Open enrollment
- Regulatory compliance
- Benefits & payroll changes
- Policy updates
- Business Continuity
- Risk assessment
- Critical event response
- Stakeholder coordination
- Supply chain continuity
- Employee safety status
- Dispatch coordination
- Operations
- Office Closures
- Travel advisories
- Power outages
- Facility updates
- Equipment malfunctions
- Shift scheduling
- Disaster Recovery
- Threat alerting
- System failure notifications
- IT team escalations
- Response coordination
- Recovery updates
- Restoration confirmation
“AlertMedia was the best solution we looked at. Easiest set up and had the most functionality.”

Mike Neighbors Director IT Infrastructure, Coca-Cola Bottling Company
“Our relationship with AlertMedia is the type of relationship vendors always say you’ll get, but you never really do. The entire AlertMedia team treats our people and business as their number one priority.”
Larry Pomykalski Director of Business Continuity & Fleet Operations, SAC Wireless
"Fabulous mass communication system that has exceeded our expectations across the board!"
Senior Manager, DHL
"We love the product! We chose AlertMedia because the product was priced right and had all the features we were looking for."
Service Desk Manager, Volkswagen Group of America
“We have had a fantastic experience with the entire AlertMedia team and having a go-to contact that knows our company, understands our goals, and is invested in our success has made for a powerful partnership beyond that of a typical vendor.”
Jennifer Saylor Manager of Customer Operations, Greyhound
“AlertMedia checks all the boxes: two-way messaging, data integrations, a strong mobile app, and a reliable product that will give you and your people peace of mind before, during, and after an emergency.”

Jon Meyer CTO, CAPTRUST
“Within 15 minutes of receiving my login, I had all 375 employees uploaded, and I was sending test messages to our employee base within seconds.”

John Hargrove CISO and SVP of IT, Franklin Mint Federal Credit Union
“During Hurricane Harvey, AlertMedia made communications with our staff so much easier.”

DeKeitra Fizgerald Claims and Safety Manager, Gulf Coast Regional Blood Center
"AlertMedia’s platform makes it easy to isolate impacted employees and quickly communicate with them based on location via texts and emails."

Tom Porter Former Director of Human Resources & Administration, Kawasaki
"AlertMedia's software is very easy to use and doesn't require IT involvement to implement or maintain which, especially as a smaller organization, was a huge selling point.
Joshua Newell Director of Service and Support, T2 Biosystems
“By consolidating all communications into one intuitive system, GSC has achieved a degree of transparency and control over dispatcher-driver communication that competitors simply can’t replicate.”

Israel Miller Dispatch Supervisor, GSC Logistics
“AlertMedia is so simple, anybody could learn how to use this platform in a matter of minutes.”

Lawrence Robert VP of Business Continuity & Risk Management, Rockland Trust
“AlertMedia goes far beyond emergency communication—it solves the challenges of communicating with a highly mobile workforce to ensure all business-critical communications get seen immediately.”

Melissa Guttman Principal of Talent, JMI Equity
“AlertMedia allowed us to upgrade our current communication system and combine it with the critical location tracking and threat intelligence capabilities we had been missing, all within a single platform.”

Mark Ellgass Global Security Analyst, International Justice Mission
“The AlertMedia team consistently goes above and beyond in its commitment to our staff’s safety and we very much appreciate it.”
Managing Director, Texas Department of Family and Protective Services
"With AlertMedia’s mobile app, I can send an emergency alert out to employees in seconds with just a click or two from my phone."

John Muller Director of Talent, Gehring Group
"With AlertMedia, we can keep our people safe and secure while also driving positive business outcomes. It's truly a win win."
Mindy Helms Director of Human Resources, Marquette Management
"I love the AlertMedia system. It is very flexible and allows me to have preset emergency templates that make it easy to send out an alert."

Joe Weiss Plant Manager, ITW Deltar Fasteners
"By using AlertMedia to automate our communications process, we are saving a significant amount of time and money—and improving efficiency.”
Director of Philanthropy Campaigns, YMCA
"AlertMedia has been a huge component in our information sharing and communication plan during the COVID-19 crisis. I can't say enough how significant it's been."

Rachel Bomeli Director of Events and Public Safety, Fox Theatre Atlanta
“Home health care workers face unique safety risks not found in traditional health care settings. AlertMedia allows us to dramatically improve the safety and security of our employees in the field.”

Kristen Husen Home Care & Hospice Director, CentraCare
"With an intuitive product backed by a phenomenal customer success team, we were up and running within hours."

Jennifer DeSchepper Human Resources Manager, Cartwright Companies
Read more
The Emergency Communication Solution Preferred by Leading Organizations
Join the thousands of world-class organizations that rely on AlertMedia for their critical communication